Pat’s Story:
A Monaghan Man, in exile in Cavan 😊, Pat’s battles with his heart health have been incredible. Sixteen stents, a defibrillator and two pacemakers later, he’s feeling the best he has in thirty years. This February he’s sharing his story to inspire others and get behind our cardiac care fundraisers – The Big Heart Appeal and 100 Miles in a Month!
“I suppose for me it all started in 2004. I was working night duty as a Mental Health Nurse in a Psychiatric Unit. It was a quite a demanding job, and night duty can be hard on the body, you’re eating and sleeping at odd times. It can also mask some of the warning signs of potential cardiac trouble.
“During one shift, I started to feel really unwell. I went for a short lie down and actually had to be woken up, I was spark out. After initial checks it was put down to tiredness and exhaustion and I was given a few days off. During that couple of days off I went fishing with my sons. We were in the tent relaxing at night time, when I felt immense pressure coming on in my chest. I was having an MI (Myocardial Infarction) – a heart attack.

Pat with his wife, and ‘rock’, Julie
“An ambulance was called. The paramedics did a great job. I was stabilised and brought to the National Coronary Care Unit at the Mater. An angiogram identified four blockages, which all needed to be stented. As soon as this was done the pressure eased.
“While dealing with the trauma during the whole incident was quite shocking and surreal, once the stents were in, I was heading home quick quickly. That’s when the realisation hits you. It’s like post traumatic stress. And cardiac rehab is so important. It had just been introduced around the time of my first attack in 2004. Although, mostly focused on physical rather than mental rehab at that time, it did help me start to understand that life wasn’t over… you could come back from this.
“One of the mistakes I made after my first heart incident was to go back to work too soon. I had a young family and felt I needed to provide for them. You think the world’s going to stop if you don’t go back to work. Over time I’ve learned your health and being there for your family is the most priceless thing, and that’s what you need to prioritise.
“In December 2004, just eight months after the first incident, I started feeling uncomfortable again. I had pins and needles and a funny sensation in my neck. I also had what I’d describe as a ‘cardiac spasm’. The cardiologist later told me it was the heart muscle beginning to stress. Soon, I was back in the Mater again for another two stents to rectify the problem.
“Over the next decade, I needed an additional stent every year to deal with my heart issues. It was the intervention of the ICU (Intensive Care Unit) teams in the Mater and Drogheda that saved me every time. I eventually gave up my Mental Health Nursing role in 2008 to help my recovery.
“I also decided to educate myself more about my condition and try recognize the symptoms as they began to arise. The cardiac rehab teams were great for that, as well as the regional cardiac care nurse, Regina Corrigan, she was a huge support. One piece of advice I would give to anyone reading this is don’t ignore what you’re body is trying to tell you – or the ‘quare feeling’ as I call it.
“What do I mean by the ‘quare feeling’? Well, it’s definitely a pre-morbid state. You become a bit irksome, a bit contrary. Maybe you’re snoring heavier, you’re restless, or in a bit of pain – you just don’t feel right. You go quiet. These are things you shouldn’t ignore. They’re like the engine management light coming on in your car… it might seem to be driving okay, but if you ignore it and continue to drive you’re doing more damage. Don’t ignore these feelings, get things sorted straight away.
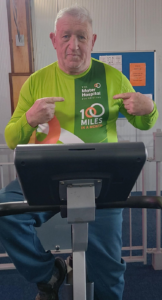
Pat taking on the 100 Miles challenge
“For me, a turning point in my condition came in 2016. After the various cardiac incidents my heart was damaged and I began to go into heart failure. I developed Pulmonary Edema – where fluid with some blood in it started to fill my lungs. One evening my wife, Julie and my daughter were coming back from an evening out. They looked in on me and could see pink bubbling around my mouth and couldn’t wake me. Another dash to ICU was needed.
“The heart team looking after me in the Mater – including Prof Keelan, Prof Mahon, Mr Sugrue, Dr Halley – reviewed my case in detail and found a solution. They operated in 2017 to put one pacemaker in the upper chamber of my heart and one in the lower. This maximized the output and stopped the ‘retro flow’ that was causing the Pulmonary Edema. In addition, they implanted a defibrillator in case my heart stopped.
“Since then, despite the odd setback during Covid, my quality of life has improved immeasurably. I’m now going to the gym five days a week. I use the bike and do my floor exercises. I honestly feel fitter than as any point since my thirties. I’ve joined the 100 Miles in a Month challenge to raise funds and give something back. It’s something that would have been unimaginable seven or eight years ago. I’m also supporting the Foundation’s Big Heart Appeal, which is raising funds to continue to improve and develop cardiac care at the hospital. I want as many as possible to benefit from the brilliant care that I did.
“These days, I get to talk to other cardiac patients about my experiences. I tell them the road can be tough, but there is often light at the end of the tunnel. And, most of all, I tell them to listen to what their body is telling them… and don’t ignore it.”
Pat Cusack, Cavan
You can support the Mater Hospital Foundation’s cardiac care fundraisers this month by clicking the links below:
Thank You!



